COVID-19 and People in Pain
By Lynn Webster, MD | November 19, 2020
On November 3, the day of the United States presidential election, more people in Pennsylvania, Ohio, and Minnesota tested positive for the coronavirus than on any other day since the pandemic began. Unfortunately, the record for the greatest number of daily coronavirus cases has been broken several times since then. How does this rampant illness impact people who suffer from chronic pain?
Chronic Pain Only Gets Worse in a Pandemic
Of all the people who have been infected by the coronavirus, people in pain have been among the most affected. People in pain are considered a high risk population. Due to the pandemic, people with pain are more likely to have increased symptoms and less likely to receive effective treatment.
The University of East Anglia (UEA) conducted a survey of 678 patients in the UK with bone, joint, and muscle pain to find out how the pandemic was affecting them. The majority of respondents said the lockdown (which was implemented in the UK because of a surge of infections) was worsening their symptoms. Mandated social isolation made them less likely to get the healthcare they needed.
Acute viral illnesses, including COVID-19, can act as triggers for chronic pain. Anxiety, too, increases pain. The fear of contracting the virus increases anxiety, thus increasing the amount of pain. Many COVID-19 patients require ICU care, and between 38% and 56% of ICU survivors later develop chronic pain.
According to a recent Journal of Pain Research editorial, members of minority groups (who are disproportionately infected with the coronavirus) have it toughest of all people with pain. The article points out that BIPOC (Black, Indigenous, and People of Color) patients are less likely than their white counterparts to receive opioid analgesia to treat their pain.
But people with pain across all demographics have had difficulty receiving the treatment they need, even before the pandemic. Physicians have chosen to abandon people in pain for several reasons, but the most common is fear of regulatory sanctions for prescribing opioids.
COVID-19 Makes Treatment More Difficult
In the effort to slow the spread of COVID-19, in-person visits to a physician have been limited, and telemedicine has replaced many visits. Going to a healthcare facility puts both patients and healthcare providers at additional risk for contracting the virus—again, worsening the situation for people with pain.
The Headache and Migraine Policy Forum, in partnership with Migraine Again, conducted a national survey of more than 1,000 migraine patients throughout the United States. Of these patients, 84 percent reported increased pandemic-related stress, with a 69 percent increase in symptoms. More than half of them postponed healthcare appointments, and nearly three-quarters refused to go to the Emergency Room when they had acute symptoms.
Therapies and diagnostic tests may require interfacing with medical personnel, so many diagnostic tests are cancelled or postponed due to the pandemic, delaying therapeutic interventions. Surgeries for people with conditions like severe spinal stenosis or arthritic knees also have been denied or delayed, while access to medication to help bridge their pain until surgery can be performed has been limited.
The most effective therapies for chronic pain involve physical therapy and cognitive behavioral therapy. Both usually require interaction with a provider which, because of the pandemic, may be refused by patients or denied by practitioners more often. People in chronic pain are often set aside because providers do not see the care they receive as critical.
Getting medication is also made more difficult by the pandemic. Unfortunately, by law, many people on opioids to control pain are unable to receive medication unless they are seen in person. In response to the pandemic, the DEA and the HHS issued a waiver to allow DEA-registered practitioners to issue prescriptions for controlled substances to patients without being seen if they are established patients.
That said, many people—including policymakers—mistakenly believe that overprescribing prescription drugs caused the opioid crisis. (Prescription opioids actually are a minor contributor to the harm caused by opioids.) The DEA is, therefore, proposing cuts in the opioid supply for the fifth consecutive year. People with chronic pain stand to be hurt the most by this.
The pandemic has affected all aspects of our lives for all of us. But those most impacted are those who have the least access to affordable care and are at highest risk if they contract the virus. Chronic pain sufferers in those ranks are hurting more than ever.
(Image: “Gone” by Benjamin Arizmendi mixed media on metal, 24″ x 30″ 2020)
Copyright © 2020 Lynn Webster, MD
Lynn R. Webster, MD, is a vice president of scientific affairs for PRA Health Sciences and consults with the pharmaceutical industry. He is author of the award-winning book, “The Painful Truth,” and co-producer of the documentary, “It Hurts Until You Die.” Opinions expressed here are those of the author alone and do not reflect the views or policy of PRA Health Sciences.
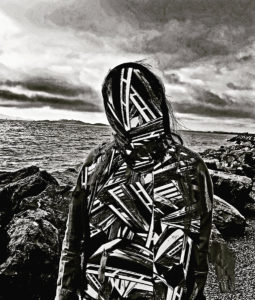
I keep coming back to this photograph. Sharp-edged cutting steel, or softly pointed bamboo ladders, crisscross panic, no foundation. An antithesis on cotton, speaks volumes toward chronic pain, never ending, lessened only occasionally. Your essay brings to light the other side of physical ailments amidst this pandemic. Thank you for posting.